LAST MILE HEALTH
Last Mile Health seeks to strengthen the fragile Liberian health system through modelling a community health worker platform at grass roots level and providing technical assistance to the National Ministry of Health.
CONTINENT
Africa

Country
Liberia
Organizational structure
Nongovernmental organization
Health focus
Primary healthcare, Maternal and child health
Areas of interest
Community health workers, Digital technologies, Last mile distribution
Health system focus
Health workforce, Information systems
CHALLENGE
Liberia’s 12 years of civil wars resulted in over 200 000 casualties, disruption of public services and the displacement of an estimated 800 000 people (Ministry of Health & Social Welfare, Republic of Liberia, 2011). The war also left the health system in a fragile state. In terms of human resources for health, as of July 2014, there were an estimated 45 physicians practicing in the public sector, a ratio of 0.01 physicians per 1,000 of the population, well below the WHO recommended threshold of 0.55 per 1,000 (Ministry of Health, Republic of Liberia, 2015). Outside the capital Monrovia, there is little or no access to health care services (Kruk et al., 2009). Of existing health facilities, 45% are without power and 13% do not have access to safe water (Ministry of Health, Republic of Liberia, 2015).

“I went back in ‘05. What I found was just utter destruction. Just 51 doctors left, all the physical destruction you’d expect from a war. Our capital where I’d grown up in Monrovia had no electricity, had no signal lights, had no running water. So you can imagine trying to rebuild a country that has a lot of odds stacked against it.”
– Dr Raj Panjabi, Co-Founder, Last Mile Health

INTERVENTION
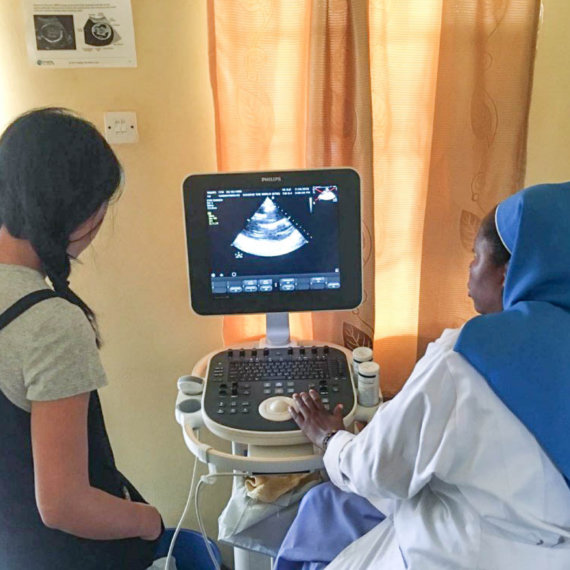
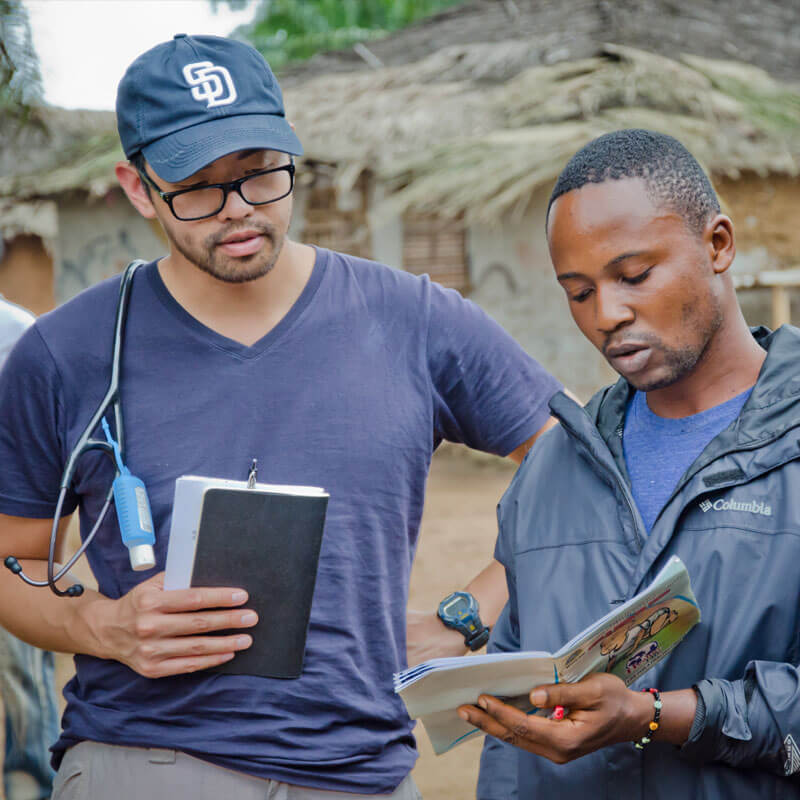
Last Mile Health (LMH) is a non-profit organization with a vision to strengthen the Liberian health system at grassroots and policy levels to increase access to care for people living in remote, hard to reach areas. It achieves this through a well-managed community health care worker (CHW) model. LMH recruits and trains CHWs in 1) community health and surveillance, 2) child health, 3) maternal and neonatal health, and 4) adult health. The training is given intensively for the first 12-months and then supplemented with annual refresher trainings. During training CHWs also do active fieldwork and upon graduation, receive ongoing clinical and managerial supervision. CHWs are equipped with diagnostic, curative and point of care tools and medication. CHWs refer patients to health facilities as needed according to established guidelines and provide point-of-care services when possible. Remuneration is performance based and linked to measures such as accuracy and efficiency. In total, LMH covers a land area of 3 925 square miles across Rivercess County, Konobo District, and Gboe-Ploe District. It has deployed 283 CHWs to cover a population of 33 664.
“We are doing something that is very transformative. I think it is going to have a significant impact. We are talking about extending access to over a million people who literally have no access to medical care… People will come up and say, ‘I’ve never seen a health worker in my whole life’. To me, that’s amazing that you can bring health care to a place that never had it before.”
– Na’im Merchant, Director of Policy and Public Partnerships, LMH
In addition to its programmatic work, LMH supports the National Ministry of Health’s Community Health Services Division by providing technical assistance to help develop policy to scale the CHW model nationwide. This is part of a broader government initiative called the National Community Health Workforce Program (NCHWP).
Over the next five years, the Liberian MOH, working with assistance from LMH, will train and deploy an estimated 4 100 professionalized CHWs and 230 supervisors to provide care for approximately 1.2 million individuals living in remote areas.

CASE INSIGHTS
The LMH case study illustrates how nongovernmental organizations can play a unique role in health systems strengthening by absorbing the experimentation risk for new innovative service delivery models, providing the financial backing and creating data systems to assess impact. It shows how country governments in turn can promote the adoption and scale of effective models. CHW programmes have significant potential to improve health care delivery to people living in rural and hard to reach areas if the programme incorporates best-practices at each stage including recruitment and selection; training; equipment and supplies; and performance management.
“I think social change gets created in two ways. One is to solve problems that have already been defined and the other is to define the problem in the first place…Embracing the consciousness to actually understand the problem in the first place and communicate around it: that remote villages are a distinct issue for health care, period.”
– Dr Raj Panjabi, Co-founder and CEO, LMH
*All images used in this layout are credited to Last Mile Health.