National Telehealth System (NTS)
NTS is a telemedicine platform that aims to improve access to specialist care among patients in geographically isolated and disadvantaged areas.
CONTINENT
ASIA
Country
PHILIPPINES
Location
National Telehealth Center, University of the Philippines Manila
Founding year
2011
Organizational structure
Government
Health focus
Primary Health Care
Actors Involved
State, Communities
Programme Focus
Service Delivery, Community Mobilisation
Governance
Logistics
CHALLENGE
In 2010, there were 4,720 barangays under the Department of Health’s (DOH) list of geographically isolated and disadvantaged areas (GIDA), identified as unserved and underserved communities. Of the 1,494 municipalities in the Philippines, 50% have GIDAs. Insufficient human resources for health undermine the ability to provide quality health care in these areas. Health professionals that remain in GIDAs are not only faced with limited financial and logistical resources but also support from other critical human resources and specialist health professionals to ensure the delivery of quality health care services.

“Telemedicine is a systems intervention, not a health information or technology intervention. I think it’s important to note that technology itself will not change things unless you change the human and the organizations around it and that’s why it’s a disruptive technology.”
– Portia Fernandez-Marcelo, MD, MPH, Project leader, National Telehealth System, Social Innovator

INTERVENTION
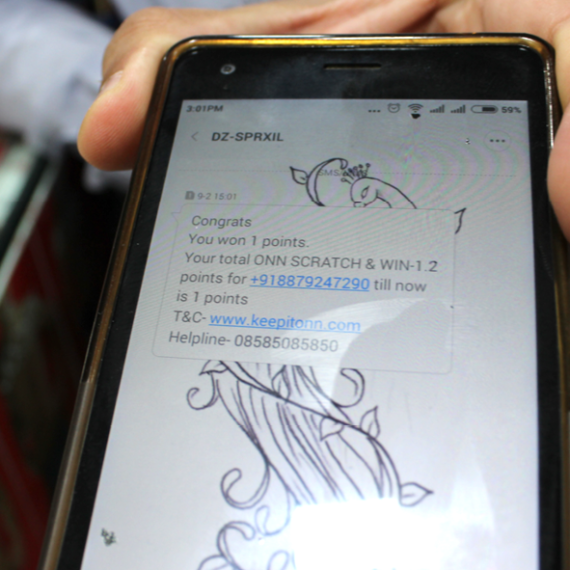
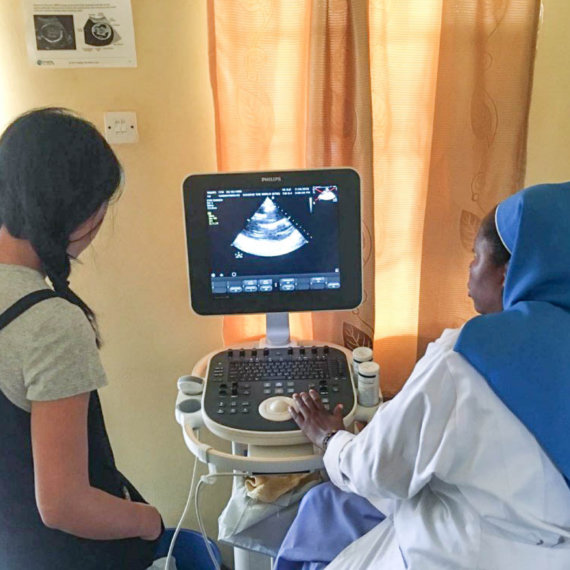
NTS serves as a platform for patients in remote and disadvantaged communities to access specialist and subspecialist care and support through their local rural health workers. The project leverages ubiquitous technology solutions such as short messaging services (SMS) or emails to improve access to specialist input for rural health workers. The innovation is in the secure referral network that the project created, linking rural health physicians to clinical specialists in selected regional hospitals nationwide. At the core of NTS is a training programme that inculcates the value of ethico-legal frameworks in the practice of telemedicine and advocates the use of locally available resources such as papel de japon (Japanese paper) and paper bills to calibrate lighting in capturing images for teledermatology. The current protocol only allows consultations or referrals for non-urgent, non-emergent cases, and has a turnaround time of 48 hours.
“I started off with a problem and finding creative solutions around that. What is most important is the humility that I don’t have all the solutions.”
– Portia Fernandez-Marcelo, MD, MPH; Project leader, National Telehealth System
NTS is used by clinicians from 175 healthcare facilities that are serving more than five million Filipinos. Since 2004, the National Telehealth Center has addressed over 2,000 teleconsultations and telereferrals coming from healthcare facilities found in GIDAs.
Nearly 800 cases were resolved directly through telereferrals and teleconsultations. This significantly reduces the potential costs to the patient for an in-person consultation with a doctor in the nearest rural health unit or hospital. After the NTS was introduced and implemented, health workers reported higher levels of motivation and feeling empowered to deliver quality health care services to their constituents, even with limited resources, through telemedicine.


CASE INSIGHTS
Physical and technological considerations and a strong network of health workers are essential in implementing NTS. A good health IT governance for transparency and direction, a cohort of clinical specialists ready to receive and respond to telemedicine consultations, well-trained health care workers, adequate health IT infrastructure, and health facility registries are just some of the elements that should be present. Communities are brought together when patients are more confident in their health care providers. Cultural and professional gaps are bridged by connecting physicians practicing in the provinces and more remote areas with clinical specialists in the regional health facilities and in the Philippine General Hospital.