BROADREACH GP DOWN-REFERRAL MODEL
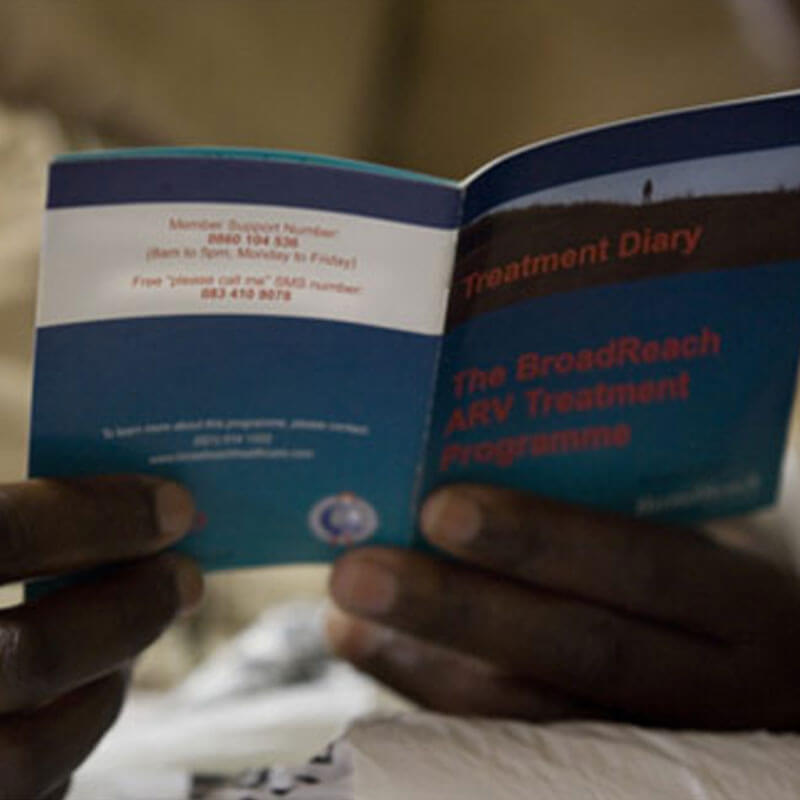
A public-private partnership model referring public sector HIV positive patients to private general practitioners. In so doing it enhances routine HIV care for patients and reduces the pressure on an overburdened public primary health system.
CONTINENT
Africa

Country
South Africa
Organizational structure
Public-private partnership between BroadReach Healthcare (private company) and the North West Province Department of Health (DOH)
Health focus
HIV
Areas of interest
Public-private partnerships, Private providers
Health system focus
Service delivery, Health care financing
CHALLENGES
HIV prevalence in South Africa rose from 0.8% in 1990 to 4.3% in 1994 (Simelela & Venter, 2014) and was at 12.2% in 2012 (Shishana et al., 2012). In addition to its heavy HIV burden, South Africa is faced with a critical shortage of doctors. In 2013, South Africa had 60 doctors per 100 000 citizens, compared to a world average of 152 doctors per 100 000 (Econex, 2015). Strain on the country’s health care system is exacerbated by large disparities between the private and public sectors. Annual per capita health expenditure is approximately US$ 140 in the public sector, serving 84% of the population, and US$ 1 400 in the private sector serving only 16% of the population (Benatar, 2013; Mayosi & Benatar, 2014). The distribution of medical specialists in the private sector is 86.5 per 100 000 compared to 11.4 per 100 000 in the public sector (Stuckler, Basu & McKee, 2011; Econex, 2015).
“If you need one clinic for 10 000 people; if we were conservative and we said we had 45 000 people… then we need 45 clinics. We have got 17 clinics. It is way too few. If we take in the GPs and utilize them as part of our system, yes we are [still] going to need the clinics but it gives us a bridge to actually deal with the patient care whilst we expand clinics.”
– Professor Variava, Clinical Head of Internal Medicine, Tshepong Hospital

INTERVENTION
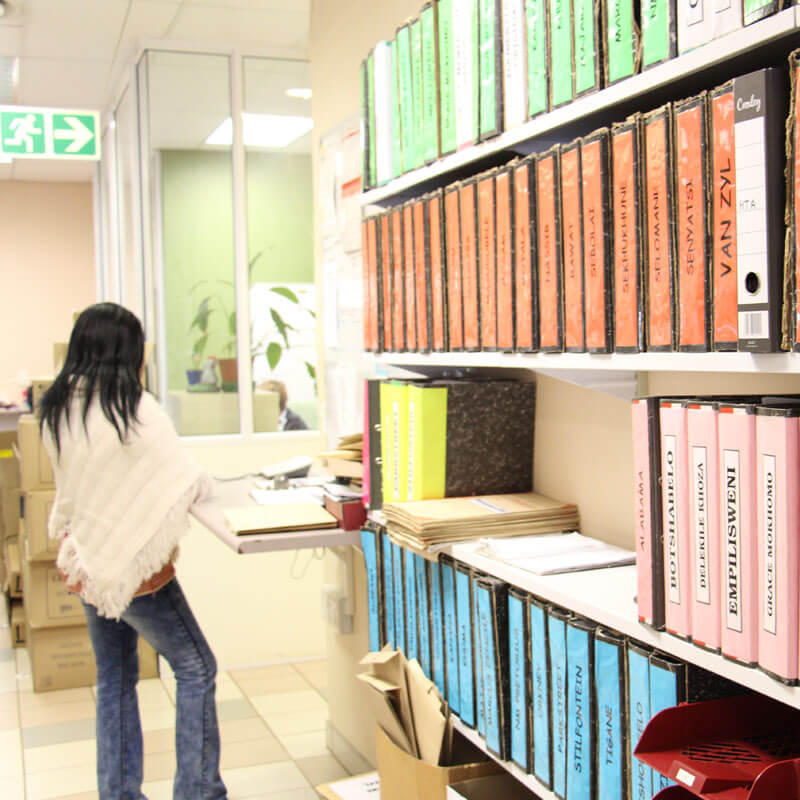
The General Practitioner Down-Referral Model (GP Model) utilizes the additional capacity of the private sector to meet gaps in the provision of health care services for HIV patients in the public sector. It enables medically stable HIV patients to be down-referred from public sector hospitals to local private general practitioners (GPs). It has been specifically constructed to provide support for the overburdened public health care system, which was struggling to cope with the large number of HIV patients needing antiretroviral therapy in South Africa. The GP Model is a public-private partnership (PPP) between BroadReach Healthcare, the North West Province Department of Health (DOH), and KOSHMED and MAIPA (two independent private general practitioner associations in the North West Province). Donor funding was provided for 10-years to cover the consultation fees of the GPs participating in the Model. These fees were fixed at a negotiated rate, which was determined with input from all partners and structured so that it would be feasible for the North West Province DOH to absorb this cost if donor funding did not continue. Ten years into the GP Model, donor funding has indeed ended and discussions are at an advanced stage for the DOH to absorb these costs as initially planned.
“I think we are achieving excellent results for a very difficult disease [HIV].”
– Private GP involved in the GP Down-Referral Model
Since the GP Model began in 2005, 4 158 patients have been transferred to private GPs for routine HIV care. In an external study conducted by Navario (2009) comparing the GP Model and primary health care clinic down-referral model (PHC), the following results were obtained: 1) the proportion of patients who remained in care at the down-referral site with suppressed viral loads was 83% and 55% in the GP Model and PHC cohorts respectively; 2) eighty-eight percent of GP Model patients had suppressed viral loads compared to 67% of PHC patients; and 3) retention on treatment was 94% among GP Model patients and 75% among PHC patients.

CASE INSIGHTS
The GP Model illustrates that down-referring by out-contracting selected health care services to private providers with additional, under-utilized capacity is a feasible mechanism to provide and increase access to quality services for public sector patients in resource-constrained environments. The GP Model also provides an example of how planning for sustainability can impact the future success of such models. Donor funding was provided for 10-years to cover the consultation fees of the GPs participating in the Model. These fees were fixed at a negotiated rate, which was determined with input from all partners and structured so that it would be feasible for the North West Province DOH to absorb this cost if donor funding did not continue. Ten years into the GP Model, donor funding has indeed ended and discussions are at an advanced stage for the DOH to absorb these costs as initially planned. As demonstrated by the GP Model, appropriate costing increases the likelihood that effective models can be successfully integrated into the public health system.
“It’s a programme that actually gets out there and works and actually affects the lives of people … When we have those breakthroughs, those moments when the stars aligned and [the] programme actually goes forward and is implemented on the ground as intended. Those are the moments that really give me the most joy because often it’s been very, very hard for us to get to that point.”
– Dr Ernest Darkoh, Co-founder BroadReach Healthcare