WHAT IS SOCIAL INNOVATION IN HEALTH?
THE CHALLENGE AHEAD OF US
In the last century, we have witnessed many astounding medical advances. Coupled with this, the public health community has made bold commitments to achieve health care for all. Despite our best human efforts, scientific progress and aspirational declarations, the lived experience of health systems and health services remain far from ideal, as millions of people in low- and middle-income countries not having access to quality affordable health services, and hence not benefiting from our advances. The time has come to turn our attention to go beyond the ‘what’ of healthcare delivery and cast attention to the ‘how’. How can we get tested and proven scientific and technological inventions to reach our most marginalised populations, and how can we ensure these communities are not mere passive recipients of our endeavours but active participants in creating their own health?
A GLOBAL VISION
The Sustainable Development Goals are calling for a renewed focus on addressing issues hindering societies from thriving. It is recognized that a new and more inclusive paradigm is required to achieve universal health coverage, in which people from different sectors, disciplines and backgrounds contribution is needed.
The Declaration of Astana (2018) provides a renewed commitment to the foundational nature of primary health care within health systems and as a pre-requisite to achieving Universal Health Coverage and the health-related Sustainable Development Goals.
Can we as a global community achieving quality, safe, comprehensive, integrated, accessible, available and affordable health care and environments in which communities are empowered?
UNDERSTANDING SOCIAL INNOVATION IN HEALTH
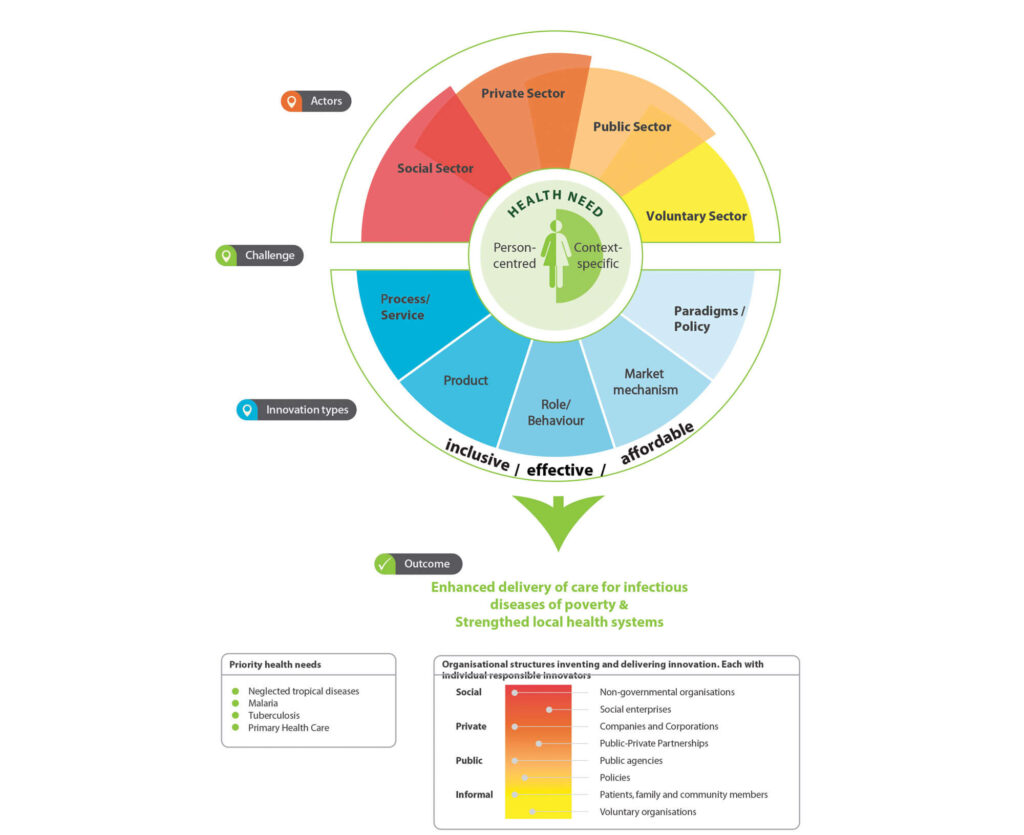
Solutions to complex problems
Social innovation gives us an alternate lens through which we can view health systems strengthening. It starts with the belief that individuals from all walks of life can be competent interpreters of their own lives and knows best how to address the problems experienced. Social innovations are merely solutions to problems. They provide creative and unconventional approaches to address complex and wicked problems which we have not been able to solve despite our best attempts. The millions of people without access to essential health services in LMICs is an example of a ‘wicked’ problem.
Innovators from all backgrounds
Social innovations can come from anywhere, designed and implemented by individuals, organizations or institutions from different backgrounds and sectors. Most often, these solutions cut across traditional silos and sit outside the traditional boxes. From our research in social innovations we have found them coming from grassroots individuals, frontline health workers, ministries of health, NGOs, for-profit companies, charities or faith-based organizations.
Forms of social innovations
Social innovation projects can take different forms. These can be: processes (e.g. reorganized care pathways); products (e.g. mobile phone applications); market mechanisms (e.g. social finance instruments); role and behavioral practices (e.g. peer-to- peer services); or new paradigms and policies. Most often, a social innovation is comprised of a combination of these forms.
Outcomes of social innovations
Social innovations achieve several outcomes:
• The solution enables healthcare delivery to be more inclusive, effective and affordable.
• The solution changes the social relationships between people and results in greater social inclusion.
• The solution empowers and builds the capacities of communities and individuals involved.
• The social innovation process reshapes institutions and thus builds greater resilience in the system.
Impact of social innovation
Social innovation is contrary from invention or traditional innovation in that it is not done in pursuit of ‘newness’ or great profit margins but with the intention of improving quality of life, achieving justice and equity, and positive social change.
Stories of Impact
A young woman who has benefited from the Central American youth support platform Joven Salud is now part of its support and volunteer network.
Young woman pays it forward by joining JovenSalud as a support and a volunteer
María Guadalupe, a 22-year-old Nicaraguan woman, learned about the online health promotion platform, JovenSalud.net, through Facebook. She was the first person in her family to go to university and entered just when her mother migrated from the country looking for new opportunities to support her daughter’s dream. María Guadalupe had to migrate to the country’s capital to attend university. The JovenSalud.net platform became a great support, especially the service “Looking for Advice?”
“I found out about JovenSalud.net through Facebook,” Maria Guadalupe said. “I wasn’t sure at first that I would like it, but I love the platform. I contacted the TeenSmart staff in my country and told them that I wanted to support and volunteer. From there, I became a leader of JovenSalud and a co-creator of the content for the new intervention ‘My Future Without Borders.’ The whole experience has been a delight!”
Learn more about JovenSalud: https://jovensalud.net/
Social innovations in health are inclusive solutions to address the healthcare delivery gap that meet the needs of end users through a multi-stakeholder, community-engaged process (Halpaap et al., 2020).
INSIGHTS FROM RESEARCH IN SOCIAL INNOVATIONS FROM LMICS
Since 2015, we have identified over 600 health projects, and selected over 50 social innovations for in-depth case study research. These social innovations came from 24 different low- and middle-income countries. The image below gives a brief snapshot of the characteristics.
FROM THE INITIAL 23 CASES OF SOCIAL INNOVATION WE STUDIED FROM 2015-2017, FIVE KEY INSIGHTS WE GAINED:
- Social innovations enhance government/public sector health delivery capacity
- Social innovations re-imagine the role of human resources for health
- Social innovations prioritize impact, agility and sustainability
- Social innovations support data driven learning and decision-making
- Social innovations outcomes extend beyond health
SOCIAL INNOVATION IN HEALTH: CASE STUDIES AND LESSONS LEARNED
WHAT IS SOCIAL INNOVATION IN HEALTH
VOICES FROM THE GLOBAL SOUTH