OPERATION ASHA
Decentralizing tuberculosis diagnosis and care through a community-based model that closes the delivery gap experienced by low-income patients in India.
CONTINENT
Asia
Country
India
Organizational structure
Nongovernmental organization
Health focus
Tuberculosis
Areas of interest
Community health workers, Last mile distribution, Digital technology
Health system focus
Service delivery, Health workforce
CHALLENGES
Operation ASHA (Op ASHA) is a community-based model aiming to improve delivery of health care services for low-income tuberculosis (TB) patients in India, and more recently Cambodia. India has the highest burden of TB globally; with 2.2 million new cases, 250 000 deaths annually and a growing number of multi drug resistant (MDR) and extensively drug resistant (XDR) TB cases (Dhanaraj et al., 2015). Although the public sector in India offers free TB services, critical challenges exist in the pre-treatment loss to follow-up and treatment adherence. For low-income communities especially, challenges arise from long commutes to health care facilities, long queues and waiting times, hidden costs to receive treatment, and missed days of work due to these access constraints.

“Keeping in mind all these challenges, Sandeep and I came up with a solution and the solution was doorstep delivery. Let’s take TB treatment to the doorsteps of the disadvantaged… So we started with basically a community-driven model and the best way to do the community-drive model was to use existing community infrastructure.”
– Dr Shelly Batra, Co-founder and President, Op ASHA

INTERVENTION
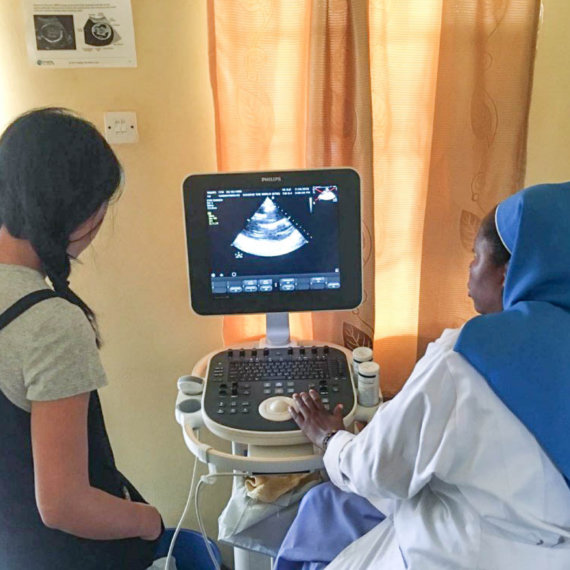
Op ASHA delivers the best practice Directly-Observed Treatment, Short-course (DOTS) strategy in a novel and accessible way. In urban areas, it does this by establishing community treatment centres in partnership with local informal providers, merchants or religious institutions. The responsibilities of these community providers entail case identification, patient enrolment, observing daily treatment adherence through DOTS and counselling. Op ASHA supplies them with the pre-packaged TB medication provided by public health facilities. These partners receive a monthly allowance to participate and also benefit from the increase in patrons visiting their shops.
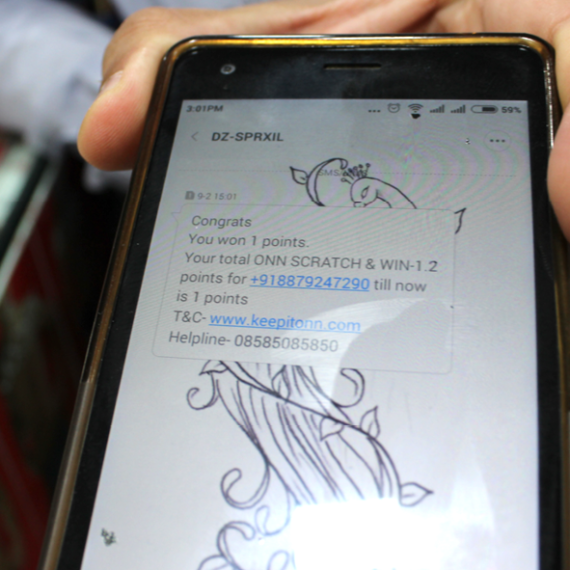
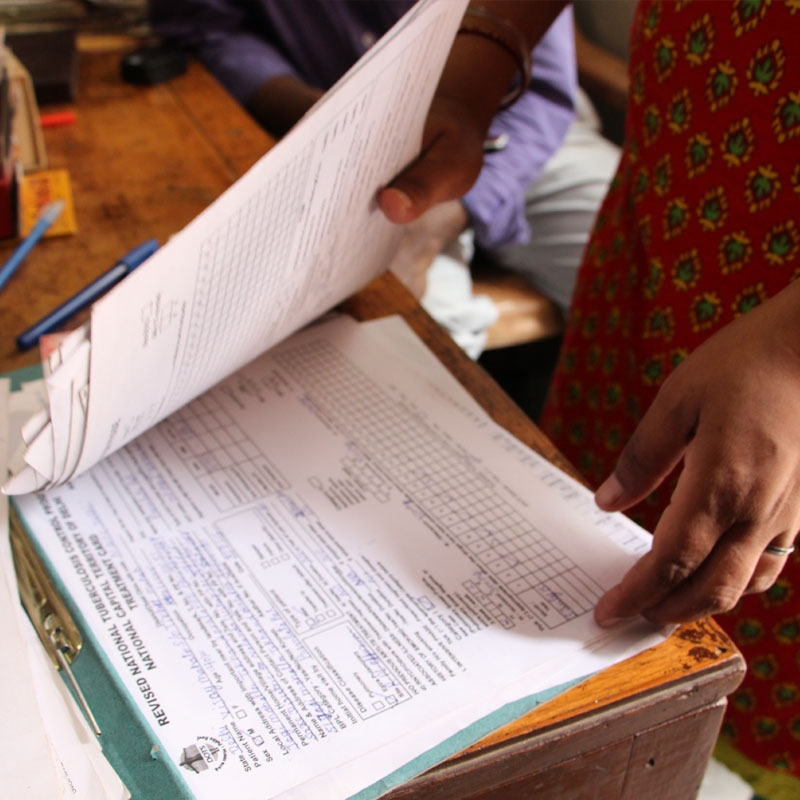
In rural areas, Op ASHA trains and employs community members to take the diagnosis and care of TB directly to patients. These community providers, often young adults, play a vital role in transporting medicines to patients’ homes in the villages, monitoring compliance and assisting patients with travel to health facilities if necessary. To promote compliance, Op ASHA has designed an internet-enabled application linked to a biometric recording system, which monitors patient drug-adherence and the effectiveness of community providers in supporting patients to receive and comply with their treatment. Through fingerprint biometric technology, every dose is monitored, records are secured and patients can be tracked across all centres.
“We take action at a single missed dose, we don’t wait for two months. We believe TB treatment means adherence has to be there. There’s no TB treatment if treatment is incomplete.”
– Sandeep Ahuja, Co-founder and CEO, Op ASHA
Op ASHA operates in eight states in India. It has 4 091 community partner distribution centres, 51 full-time staff and 126 community providers.
Op ASHA reports that 6.2 million individuals in India have been reached and have received TB education and 41 000 patients have successfully completed TB treatment. In addition, 198 MDR-TB cases have been identified and enrolled on treatment. Op ASHA’s average treatment success rate is 88% and shows a default rate of less than 3%.


CASE INSIGHTS
The Op ASHA case study illustrates how trained members from low-income communities could effectively overcome the last-mile delivery gap in TB care by extending services beyond the traditional health care facility. Clear incentives and targets motivate community workers while also ensuring that TB patients complete their treatment. It also shows how innovative nongovernmental organizations can play a role in creating effective models to complement public sector health care service delivery.
“So what we have done is this, we’ve utilized the community to bridge the gap between the disadvantaged and the government infrastructure. We provide the vital link between the two.”
– Dr Shelly Batra, Co-founder and President, Op ASHA