DRUG SHOP INTEGRATED MANAGEMENT OF CHILDHOOD ILLNESS
A pilot programme to assess the feasibility and effectiveness of engaging private sector drug shop owners in the provision of care to children under five.
CONTINENT
Africa

Country
Uganda
Organizational structure
Inter-university collaboration
Health focus
Maternal and child health, Malaria
Areas of interest
Private providers
Health system focus
Service delivery
CHALLENGES
The Drug Shop Integrated Management of Childhood Illness project is a collaborative research initiative. Structured as a pilot programme, it aims to assess the feasibility and effectiveness of engaging private sector drug shop owners in the provision of care to children under five, living in low-income areas in Uganda, particularly for treatment of malaria, diarrhoea and pneumonia. These three diseases combined are responsible for three quarters of deaths in children under five (Liu et al., 2012). Studies have found that timely community case management of malaria can reduce mortality by 60%; early treatment with oral rehydration salts can prevent 90% of deaths caused by acute watery diarrhoea; and providing antibiotic treatment in the case of pneumonia can result in a 70% reduction in mortality (Sirima et al., 2003; Munos, Walker & Black, 2010; Sazawal & Black, 2003).

“[The] biggest lessons are that solutions are available all around us and we can work with what is on the ground … Particularly if we are able to do this at the grass root [level], we should be able to see the solutions.”
– Dr Phyllis Awor, Primary Researcher
INTERVENTION
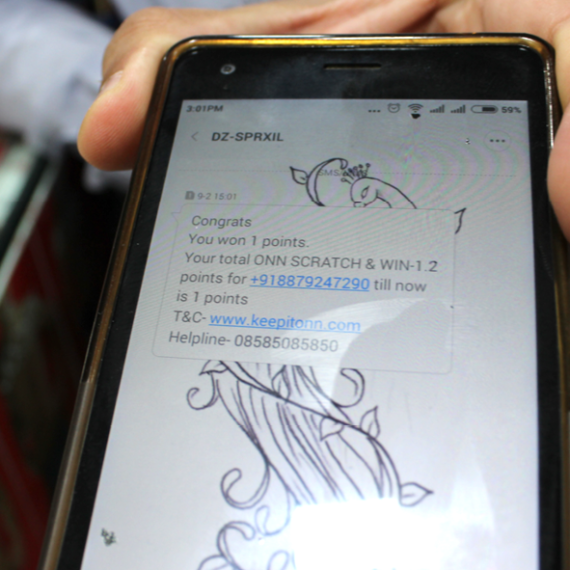
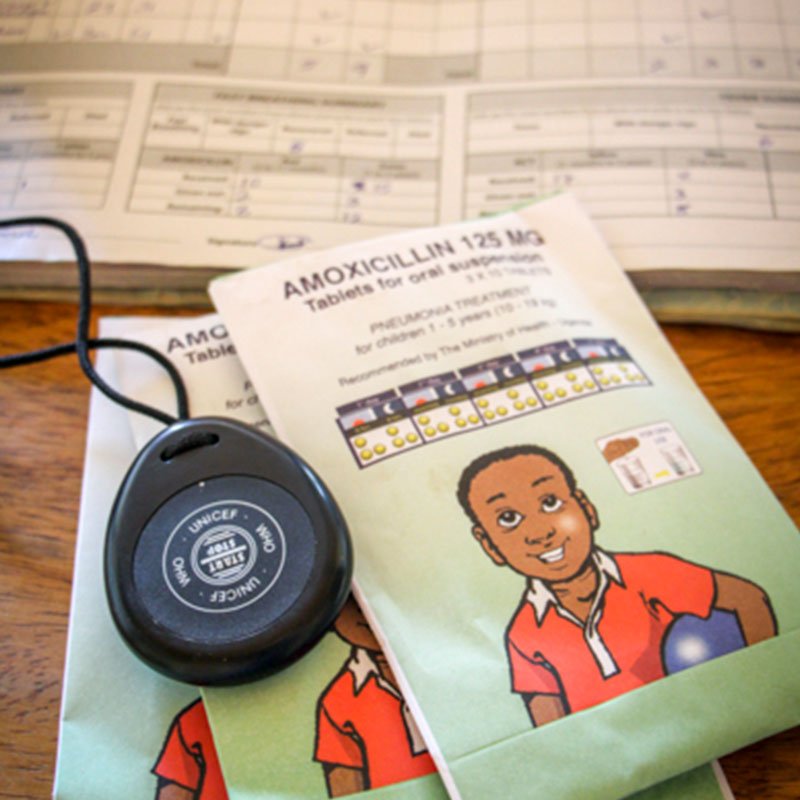
In Uganda, up to 63% of parents seek care for their febrile children primarily from private clinics and drug shops (Rutebembera et al., 2009; Awor et al., 2012). Drug shops are small private outlets that offer over-the-counter medicines and supplies for common illnesses, particularly in rural and hard-to-reach areas. In 2010, Uganda had 6 636 registered drug shops and many more unregistered ones primarily serving the population residing in rural areas (Uganda Bureau of Statistics (UBOS) & ICF International Inc., 2012). The project selected a group of drug shop owners and provided them with integrated community case management (iCCM) training, appropriate diagnostics equipment (e.g. respiratory timers and malaria rapid diagnostic tests), and subsidised medication supplies.
“It excites us a lot that we’ve shown a way to engage with this group of drug shops and actually harness their potential for improving outcomes in child health.”
– Dr Phyllis Awor, Primary Researcher
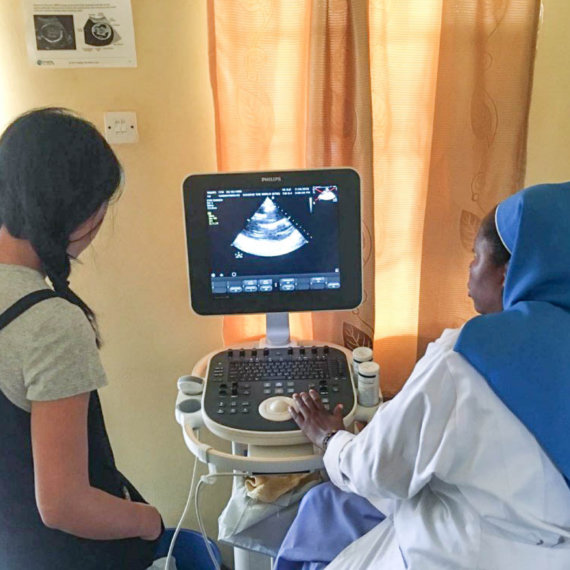
All participating drug shop owners received five days of training in iCCM and received their practical experience at local public health facilities. Accredited district health officials provided all training, and at regular intervals a supervisor and the district drug inspector would conduct visits to the shops to assess treatment provision. Referral systems were put in place to facilitate drug shop owners referring children with severe conditions to the local public health facility. A campaign was also run to increase the awareness and knowledge of the local community around the type and cost of services they could expect from accredited health facilities. Research was initially conducted using information from 7667 children visits occurring across 40 drug shops, and is currently ongoing.


CASE INSIGHTS
This case study illustrates that activities intended to strengthen the technical capacity and quality delivered by the health care system need to extend beyond the public sector to include private sector providers. This is particularly appropriate in countries like Uganda, with high out-of-pocket health expenditure, and where low-income patients regularly first seek care from private facilities. This case also highlights the opportunity for more collaboration between academics, policy makers, regulators and entrepreneurs in the design of implementation strategies. More comprehensive and holistic strategies help ensure that an effective innovation is financially sustainable and amenable to widespread adoption.
“When you see a sick child getting better or a mother actually telling you, ‘Thank you’ … You listened to this drug seller actually thanking me four times. That’s the joy that it brings to us. … Changing some people’s lives – the business life and also particularly improving the health of the community – that’s what brings the biggest joy.”
– Dr Phyllis Awor, Primary Researcher